In recent years, medical headlines have featured frightening new challenges, ranging from Ebola to Zika and antibiotic-resistant bacteria. While these crises rightly raise public concern, real progress has been made in combatting longstanding global health threats. Worldwide HIV/AIDS deaths declined by nearly 46 percent between 2006 and 2016, while preventable diseases like diphtheria and measles caused over two-thirds fewer fatalities over the same period. As a result, people around the world are living longer and more healthily than ever before.
This success is uneven, however. Health outcomes vary dramatically by country, indicating vast disparities in conditions and care across the globe. Ninety-five percent of tuberculosis cases occur in the developing world, for example, while children younger than 5 years old are 14 times more likely to die in sub-Saharan Africa. While these differences reflect a host of cultural and geographical factors, they may also relate most to one key indicator: the availability of medical professionals and resources.
We set out to determine the prevalence of health resources and the people who provide them across the world. To do so, we studied data from the Organisation for Economic Co-operation and Development to learn which countries make care widely available, and which struggle with too few providers. Our results reveal deep inequalities at the heart of global health trends and the challenges confronting physicians and medical advocates throughout the world.
Doctor Disparities

Explore the above interactive by selecting the countries you wish to examine.
Note: Percentages shown signify the percentage difference in the number of physicians between each country's initial and most recent reporting years.
When we consider the number of reported physicians in each country over time, we see significantly different trajectories among nations. Countries boasting nationalized public health care systems saw the greatest increase in reported physicians relative to their population. Denmark’s doctor representation more than doubled between 1980 and 2014, as did Columbia’s from 1990 to 2014. Conversely, the U.S. saw a difference of a little over 21 percent between 1993 and 2014, the period in which data are available.
Few countries witnessed significant periods of decline in our data, though they share a Soviet history. While Estonia’s doctor representation has increased substantially since 1960, it’s actually down since its peak in 1984. Russia, meanwhile, saw its concentration of doctors continue to increase through 2010, though its numbers have dropped significantly since. The Russian medical system has attracted intense criticism of late, perhaps discouraging new entrants to the field.
Physicians: A Gendered Profession?
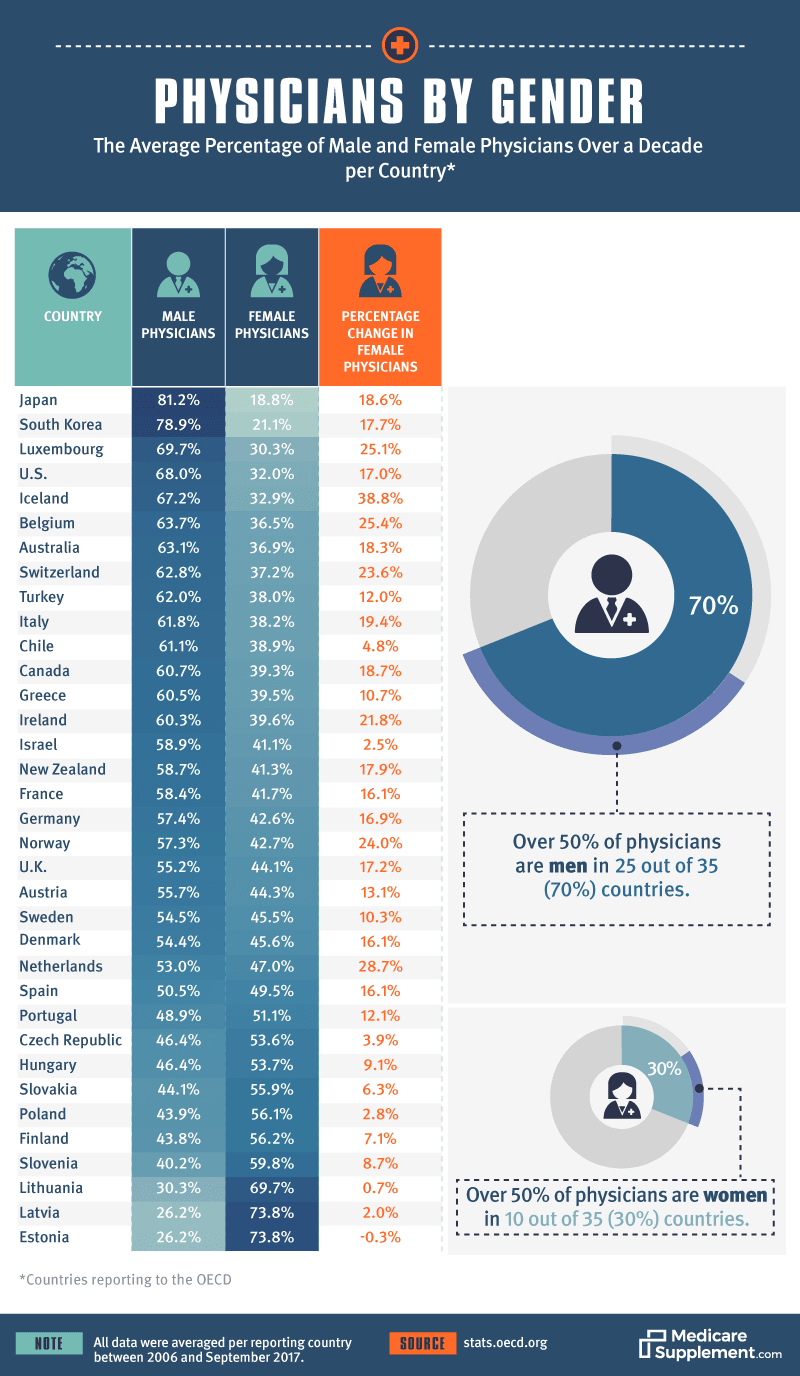
One means to increase the count of doctors is to create equal opportunity to enter the profession – for candidates of any gender. Unfortunately, many nations with enviable health indicators have less-than-desirable records on gender equity in the field. Japan and South Korea, for instance, boast notably long life expectancies for all citizens, yet only about 1 in 5 practicing doctors in each country is female. In the U.S., the gap is only slightly smaller, with women representing approximately a third of the current doctor workforce.
While physicians are mostly male in the vast majority of nations, some interesting outliers also emerged. Former Soviet bloc countries are particularly likely to see female practitioners, which some medical researchers have attributed to USSR government’s efforts to encourage female participation in the medical community. Finland also boasts one of the highest rates of practicing female physicians. The country has long had a progressive record of gender equity, including becoming the first nation in Europe to allow women to vote.
Care Providers by Country

Doctors aren’t the only medical professionals worth considering: Nurses and midwives also serve important roles in each nation’s health care system. Midwifery services are quite accessible in the nationalized health care systems of the Nordic states, which explains their concentration in Iceland, Sweden, and Norway. Australia, however, leads all countries in this category. This is likely due to the county’s 2012 decision to alter its requirements to practice in the field, which has seen occasional growth in the profession since that year.
Nurses are also distinctly well-represented in the Nordic countries, though they are far more numerous than either midwives or physicians in virtually every country studied. Unfortunately, many nations with apparent doctor shortages also have a low proportion of nurses: Indonesia and South Africa were near the bottom of the scale for both. This suggests a general lack of care available at every level, a troubling statistic for any nation.
Where People Get Well

Hospitals can indicate a country’s ability to meet its population’s medical needs, and dramatic variations are visible among developed and developing nations alike. Japan boasts the most hospitals per capita, which may contribute to growing concerns about the fiscal sustainability of the system in the years to come. Despite its universal health care system, few of Japan’s hospitals are government-run. By contrast, virtually all hospitals in countries like Iceland and Canada are publicly owned, unifying insurance and care under government auspices.
Relative to other developed nations, the U.S. can claim relatively few hospitals per capita. Perhaps this is due to a recent trend of mergers between medical institutions to reduce costs. Still, a comparatively limited number of beds may pose a problem for American hospitals in the future. The U.K., which has the same rate of beds available, faced consistent shortages in 2017.
Room to Recover

Explore the above interactive by selecting the countries you wish to examine.
Note: Percentages shown signify the percentage difference in the number of physicians between each country's initial and most recent reporting years.
A closer look at hospital bed availability reveals some remarkable instances of decline, both in America and elsewhere. The U.S. has seen its number of beds per capita decline nearly 70 percent since 1960, while Canada witnessed a similar trend. Perhaps this reflects improvement in some ways, however. The average length of hospital stays worldwide has consistently contracted over time, an indication of increased care efficiency. As a result, fewer beds may be required at any given moment.
Asia seems like the primary source of hospital bed growth in recent history, with South Korea and China both building more hospital beds per capita. Some have suggested China is actually too dependent on its hospitals, urging a more frequent use of general practitioners to combat treatable and preventable diseases.
Immunization by Nation

Regarding vaccination prevalence, Eastern Europe can claim better rates than many of its wealthy Western neighbors. In fact, the four countries with the most thorough child vaccination records hail from that region. Conversely, the U.S. has only a mediocre standing on the international stage, with more than 7 percent of its children going unvaccinated for measles, hepatitis B, and influenza. This may be due to a small but vocal minority of American parents who resist vaccinating their children, despite overwhelming evidence of their safety.
Still, other developed nations had even lower child vaccination rates, including Sweden, the Netherlands, and France. Perhaps this trend will reverse as measles outbreaks continue to occur on the European continent. The French government recently took Italy’s lead in legally requiring its citizens to vaccinate their children, beginning in 2018.
Your World of Health Care
As our results make clear, health care and its outcome differ vastly among countries, often in fascinating ways. These contrasts result from each nation’s particular cultural and historical context, as well as the resources with which it’s endowed. Still, much progress can and must be made to bring affordable and effective care to every corner of the globe. By analyzing key indicators as we’ve done in this project, governments and the medical community can unite around solutions that keep more humans healthy – wherever they may live.
Methodology
To prepare this project, we assessed international health care data from the Organisation for Economic Co-operation and Development in September 2017. All data included represent the most extensive and recent information available for each country, though data availability differed significantly among nations.
Fair Use Statement
Want to spread the word of health resources around the world? Feel free to share our information and assets for noncommercial purposes. We’re all for a little healthy debate. When you do, please attribute us fairly by providing a link to this page.
